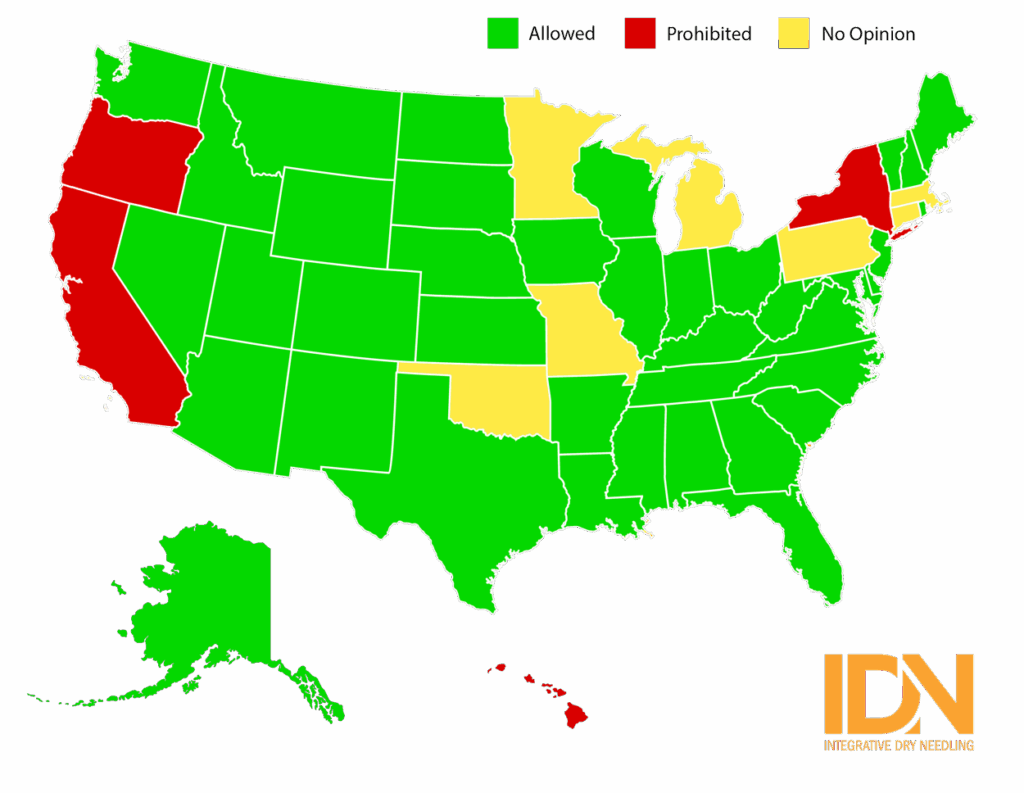
U.S. State Dry Needling Scope of Practice Decisions (APTA reference)
Resource: Federation of State Boards
The American Physical Therapy Association states that Dry Needling is within the scope of practice for a Physical Therapist. Several other health professions cite that dry needling is within their specific scope of practice as well. There are however, specific U.S. state rules, regulations and guidelines that do not permit the practice of dry needling. It is your responsibility to know, understand and practice within the specific rules, regulations and guidelines of your state, jurisdiction and professional license.
The Integrative Dry Needling Institute LLC is solely an educational resource to provide the knowledge and technical skills necessary to deliver safe and effective dry needling treatment. The Integrative Dry Needling Institute LLC does not make policy, claims, or interpretation on professional licensure or scope of practice. The Integrative Dry Needling Institute LLC encourages all participants to contact their licensing board for official positions and rulings related to the practice of dry needling.
May 2008, the Alabama Board of Physical Therapy determined that dry needling is within the scope of physical therapy practice. Alabama’s position on Physical Therapist Assistants performing dry needling.
In April 2012, the Alaska PhysicalTherapy and Occupational Therapy Board approved dry needling by physical therapists.
On April 25th, 2014 the Arizona physical therapy statute was ammended to include dry needling within the physical therapy scope of practice.
R4-24-313. Professional Standards of Care and Training and Education Qualifications for Delivery of Dry Needling Skilled Intervention
A. Effective July 1, 2015 and in accordance with A.R.S. § 32-2044(25), a physical therapist shall meet the qualifications established in subsection (C) before providing the skilled intervention “dry needling”, as defined in A.R.S. § 32-2001(4).
B. A physical therapist offering to provide or providing “dry needling” intervention shall provide documented proof of compliance with the qualifications listed in subsection (C) to the board within 30 days of completion of the course content in subsection (C) or within 30 days of initial licensure as a physical therapist in Arizona.
C. Course content that meets the training and education qualifications for “dry needling” shall contain all of the following:
1. The course content shall be approved by one or more of the following entities prior to the course(s) being completed by the physical therapist.
a. Commission on Accreditation in Physical Therapy Education,
b. American Physical Therapy Association,
c. State Chapters of The American Physical Therapy Association,
d. Specialty Groups of The American Physical Therapy Association, or
e. The Federation of State Boards of Physical Therapy.
2. The course content shall include the following components of education and training:
a.Sterile needle procedures to include one of the following standards:
-The U.S. Centers For Disease Control And Prevention, or
-The U.S. Occupational Safety And Health Administration
b. Anatomical Review,
c. Blood Borne Pathogens
d. Contraindications and indications for “dry needling”,
3. The course content required in subsection (C) of this Section shall include, but is not limited to, passing of both a written examination and practical examination before completion of the course content. Practice application course content and examinations shall be done in person to meet the qualifications of subsection (C).
4. The course content required in subsection (C) of this subsection shall total a minimum of 24 contact hours of education.
D. The standard of care for the intervention “dry needling” includes, but is not limited to the following:
1 “Dry needling” cannot be delegated to any assistive personnel.
2 Consent for treatment for the intervention “dry needling” is the same as required under R4-24-301.
3 Documentation of the intervention “dry needling” shall be done in accordance with R4-24-304.
On May 28, 2009, the Arkansas State Board of Physical Therapy ruled that dry needling is within the scope of physical therapy practice.
September 2013: Colorado Governor signs into law that Dry Needling is in the scope of practice for Physical Therapy.
To be deemed competent to perform dry needling, a physical therapist must successfully complete a formalized course of study provided by a qualified licensed healthcare provider that:
-Includes a minimum of fifty (50) hours of education of which forty hours must be in-person education. The education may be broken up into more than one part. A physical therapist is permitted the limited practice of dry needling once the physical therapist has completed thirty hours, as long as such practice is confined to the scope of the education already successfully completed. All parts of this education must be successfully completed within four (4) years.
The formalized course of study may be completed during the physical therapist’s entry level education. To apply this education to the requirements, the remaining parts of the education must be successfully completed within four (4) years of the date of original licensure.
If the physical therapist has not completed at least fifty (50) hours of dry needling training within four (4) years, then the licensee must stop performing dry needling at any level until the licensee has completed at least fifty (50) hours.
A physical therapist who meets the requirements must maintain documentation regarding the successful completion of these requirements and shall provide the documentation upon request by the Board.
Novemember 2009: The District of Columbia Board of Physical Therapy approved dry needling to be within the scope of physical therapy practice.
July 1st. 2014: Delaware passed a bill that redefines and expands the ‘practice of physical therapy’ and ‘athletic training’ to include the use of dry needling treatment.
15.4.1 Dry needling is “an intervention that uses a thin filiform needle to penetrate the skin and stimulate underlying muscular tissue, connective tissues and myofascial trigger points for the management of neuromusculoskeletal pain and movement impairments; is based upon Western medical concepts; and requires a physical therapy examination and diagnosis.” 24 Del.C. §2602(6). Dry needling is within the scope of practice for a Physical Therapist. 24 Del.C.§2602(10)(a). It is not in the scope of practice for Athletic Trainers, Physical Therapy Assistants or Physical Therapy Aides.
15.4.2 Requirements for Physical Therapists to perform dry needling:
15.4.2.1 Dry needling may be performed by a licensed Physical Therapist who meets the requirements of subsection 15.4.
15.4.2.2 The Physical Therapist shall have no less than 2 years of active clinical experience in the treatment of patients as a licensed Physical Therapist and shall hold a current license in good standing.
15.4.2.3 The Physical Therapist shall have current CPR certification by the American Red Cross, American Heart Association, National Safety Council or other agency approved by the Board and posted on the Division of Professional Regulation’s website.
15.4.2.4 Dry needling shall be performed directly by the Physical Therapist and shall not be delegated.
15.4.2.5 Dry needling shall be performed in a manner that is consistent with generally accepted standards of practice, including clean needle techniques and the bloodborne pathogen standards of the Occupational Safety and Health Administration (“OSHA”).
15.4.2.6 Dry needling is an advanced procedure that requires specialized training. A Physical Therapist shall not perform dry needling in Delaware unless he or she has and maintains documented proof of completing a Board-approved training program on dry needling.
15.4.2.6.1 The program shall be a minimum of 54 hours, which shall be completed within no more than two years;
15.4.2.6.2 The Physical Therapist shall successfully complete the minimum passing criteria for the dry needling program; and
15.4.2.6.3 The Physical Therapist shall only utilize the specific techniques for which he or she has demonstrated competency.
15.4.3 Physical Therapists who are performing dry needling at the time of enactment of this regulation, and who have completed 25 hours of dry needling education, may continue to practice dry needling, upon submission of proof of experience and education to the Board. Such Physical Therapists shall complete the required 54 hours of education within two years after enactment of this regulation.
As of July 1st 2020, Physical Therapist in the state of Florida gained the legal right to perform dry needling. Click here for more.
On May 12, 2011 the Governor of Georgia signed the Bill into law effective July 1, 2011. Georgia became the first state in the United States where dry needling became part of the Physical Therapy Statutes. Click here for guidelines.
In February 2018, the Idaho Board of Physical Therapy approved dry needling by physical therapists. Click here for guidelines
Effective 8-25-17 Dry needling is in the scope of a Physical Therapist’s practice, however, they need to meet the legal requirements as set by the board.
Sec. 1.5. Dry needling. (a) For the purpose of this Act, "dry needling", also known as intramuscular therapy, means an advanced needling skill or technique limited to the treatment of myofascial pain, using a single use, single insertion, sterile filiform needle (without the use of heat, cold, or any other added modality or medication), that is inserted into the skin or underlying tissues to stimulate trigger points. Dry needling may apply theory based only upon Western medical concepts, requires an examination and diagnosis, and treats specific anatomic entities selected according to physical signs. Dry needling does not include the teaching or application of acupuncture described by the stimulation of auricular points, utilization of distal points or non-local points, needle retention, application of retained electric stimulation leads, or other acupuncture theory. (b) A physical therapist or physical therapist assistant licensed under this Act may only perform dry needling after completion of requirements, as determined by the Department by rule, that meet or exceed the following: (1) 50 hours of instructional courses that include, but are not limited to, studies in the musculoskeletal and neuromuscular system, the anatomical basis of pain mechanisms, chronic and referred pain, myofascial trigger point theory, and universal precautions; (2) completion of at least 30 hours of didactic course work specific to dry needling; (3) successful completion of at least 54 practicum hours in dry needling course work; (4) completion of at least 200 supervised patient treatment sessions; and (5) successful completion of a competency examination. Dry needling shall only be performed by a licensed physical therapist or licensed physical therapist assistant. Full practice act
(1) A physical therapist may apply dry needling specific education hours completed within the entry-level education program toward the fifty (50) hour requirement. The physical therapist must complete any remaining education hours to reach a total of fifty (50) hours prior to providing dry needling services.
(2) The physical therapist bears the burden of proof of sufficient education and training to ensure competence with the treatment or intervention. Education courses that meet the requirements of 842 IAC 1-7-5 satisfy this requirement.
(3) If requested by the board or a member of the public, the physical therapist providing dry needling services shall provide documentation of completion of the training required by this rule.
(4) Failure to provide written documentation to the board in compliance with this requirement shall be deemed prima facie evidence that the physical therapist is not competent and shall not be permitted to perform dry needling.
(5) Dry needling shall be performed directly by the physical therapist and shall not be delegated.
On January 14, 2016, the Iowa Board of Physical & Occupational Therapy issued a Ruling on the Petition for Declaratory Order and concluded that dry needling is within the scope of physical therapy practice as defined in Iowa Code section 148A.1(1)(b).
Dry needling was added to the Kansas statute on May 13, 2016 after Governor Brownback signed the bill. State requirements
KRS 327.010(1) defines “physical therapy,” in part, as “the use of selected knowledge and skills … invasive or noninvasive procedures with emphasis on the skeletal system, neuromuscular, and cardiopulmonary function.” There is nothing in KRS Chapter 327 to prohibit a credential holder from performing dry needling so long as he or she has the requisite training, expertise, and experience to perform this function.
Pursuant to 201 KAR 22:053 Section 3, physical therapist assistants in Kentucky can provide physical therapy services under the supervision and direction of a physical therapist who has the requisite education, training and experience relating to those services.
That stated, the Kentucky Board of Physical Therapy recognizes that both the American Physical Therapy Association and Federation of State Boards of Physical Therapy have cautioned physical therapist assistants from engaging in dry needling, as they are not trained in the same competencies that qualify physical therapists to perform these services. Prior to performing dry needling services, the Board recommends that the physical therapist assistant seek guidance on this issue by reviewing the Analysis of Competencies for Dry Needling by Physical Therapists Final Report located at: http://www.apta.org/StateIssues/DryNeedling/.
In May 2011, the Louisiana Board of Physical Therapy issued standards of practice for the utilization of dry needling techniques, which formally established dry needling in the scope of practice of a physical therapist.
La. Admin. Code tit. 46, § LIV-311
In June 2016, the Maine Board of Examiners in Physical Therapy ruled that dry needling is within the scope of physical therapy practice.
In 1984, the Maryland Board of Physical Therapy Examiners was the first physical therapy board in the US that approved dry needling by physical therapists. State practice info.
In September 2012, the Mississippi Attorney General issued a legal opinion that “the Physical Therapy Board acted within the scope of its authority when promulgating the proposed rule including the use of needles for therapeutic treatment as a technique within the scope of the statutory definition of the practice of physical therapy. Practice guidelines
In May 2011, the Montana Board of Physical Therapy determined that dry needling is within the scope of physical therapy practice. More info.
In June 2011, the Nebraska Board of Physical Therapy decided that “a Nebraska licensed physical therapist may perform dry needling as long as he/she can competently perform such a procedure. This does not include physical therapy assistants”.
On June 5, 2020, the Nevada Legislative Commission approved the attached regulation prescribing the qualifications required for physical therapists to perform dry needling. In summary, the qualifications include the completion of at least 150 hours of certain didactic education and training in dry needling, and submission of documentation to the Nevada Physical Therapy Board. This education requirement includes at least 25 hours of didactic education and training provided through a postgraduate course of study that requires the successful completion of in-person written and practical examinations.
In March 2002, the New Hampshire Physical Therapy Governing Board determined that dry needling is within the scope of physical therapy practice.
Learn about our new 3-course package to achieve your states requirement HERE.
P.L. 2021,c.382 was signed by Governor Murphy on January 18, 2022 which permits physical therapists to perform dry needling under certain circumstances. The law becomes effective 90 days from January 18, 2022. Under this statute a licensed physical therapist must complete a continuing education and competency program approved by the New Jersey State Board of Physical Therapy Examiners. The law requires board approved dry needling continuing education and competency programs, which include at least 40 hours of academic instruction, attendance in person by a physical therapist, and the ability to complete the program in no more than two years. The programs are also required to include a minimum of 40 hours in practical hands-on instruction, under the direct supervision of a licensed physical therapist who has a minimum of five years of clinical experience in the performance of dry needling or by a physician licensed to practice medicine and surgery in this State, in the application of technique of dry needling. Licensees must complete a total of 80 hours from Board Approved dry needling continuing education and competency programs to qualify to practice dry needling in New Jersey. The Board approved dry needling continuing education and/or competency courses/programs at its May 24, 2022 meeting- go to Continuing Education Tab on the left side of the Board’s homepage. Then click on February 1, 2022 thru January 31, 2026 under Approved Continuing Education Course Lists. If you complete a course/program and it is not approved by the Board, it will not be in compliance with the law. Please check the Board’s website for updates regarding dry needling and dry needling continuing education and/or competency programs under Continuing Education and FAQ.
In 1999, the New Mexico Physical Therapy determined that dry needling is within the scope of physical therapy practice.
On December 7, 2018, the North Carolina Supreme Court upheld the Physical Therapy Board’s declaratory ruling affirming that dry needling constitutes physical therapy and falls within the scope of physical therapy in North Carolina.
In May 2013, the North Dakota Physical Therapy Board approved dry needling to be within the scope of physical therapy practice.
In January 2007, the Ohio Occupational Therapy, Physical Therapy and Athletics Trainers Board determined that dry needling is within the scope of physical therapy practice. As with any specialized procedure, the physical therapist must have training and demonstrate competency in the modality. The manner in which the training is obtained and competency demonstrated are not addressed in the Practice Act. The PT Board recommends you contact the OPTA for approved coursework in dry needling at www.ohiopt.org .
In May 2012 the Rhode Island Board of Physical Therapy approved dry needling by physical therapists.
In October 2004, the South Carolina Board of Physical Therapy Examiners determined that dry needling is within the scope of physical therapy practice. Physical Therapists may use the procedure if properly trained and performed within the standard of care. It is the professional responsibility of each licensee to ensure they are properly trained and competently able to do the procedure.
The board may approve a course of study in dry needling that meets the
following criteria:(1) The course of study shall include:(a) Surface anatomy as it relates to underlying tissues, organs, and other structures, including variations in form, proportion,
and anatomical landmarks;
(b) Both emergency preparedness and response procedures related to secondary physiological effects or complications with dry
needling;
(c) Both emergency preparedness and response procedures related to secondary emotional effects or complications associated
with dry needling;(d) Standards for dry needle handling;(e) Factors influencing safety and injury prevention;(f) Personal protection procedures and techniques as related to dry needling;(g) Theoretical basis for dry needling;(h) Theoretical basis for combining dry needling with other interventions;(i) Secondary effects or complications associated with dry needling on other systems;(j) Theoretical basis of pain sciences, including anatomy, physiology, pathophysiology, and relation to body structures and
function;(k) Indications, contraindications, and precautions related to dry needling;(l) Palpation techniques as related to dry needling;(m) Needle insertion techniques;(n) Needle manipulation techniques;(o) Physiological responses to dry needling; and(p) Solid filament needles;(2) The majority of the course of study shall be in-person. Courses held entirely online or by other distance learning will not
satisfy this requirement; and
(3) The physical therapist may only perform dry needling on the parts of the body included in the course of study.
Source: 45 SDR 9, effective August 1, 2018. General Authority: SDCL 36-10-52.Law Implemented: SDCL 36-10-52.
New Rule: 1150-01-.22 Dry Needling
(1) In order to perform dry needling, a physical therapist must obtain all of the educational instruction described in paragraphs (2)(a) and (2)(b) herein. All such educational instruction must be obtained in person and may not be obtained online or through video conferencing.
(2) Mandatory Training – Before performing dry needling, a practitioner must complete educational requirements in each of the following areas:
(a) Fifty (50) hours of instruction, to include instruction in each of the four areas listed herein, which are generally satisfied during the normal course of study in physical therapy school:
(b) Twenty-four (24) hours of dry needling specific instruction.
(i) Dry needling technique;
(ii) Dry needling indications and contraindications;
(iii) Documentation of dry needling;
(iv) Management of adverse effects;
(v) Practical psychomotor competency; and
(vi) Occupational Safety and Health Administration’s Bloodborne Pathogen Protocol.
(3) A newly-licensed physical therapist shall not practice dry needling for at least one (1) year from the date of initial licensure, unless the practitioner can demonstrate compliance with paragraph (2) through his or her pre-licensure educational coursework.
(4) Any physical therapist who obtained the requisite twenty-four (24) hours of instruction as described in paragraph (2)(b) in another state or country must provide the same documentation to the Board, as described in paragraph (2)(b), that is required of a course provider. The Board or its consultant must approve the practitioner’s dry needling coursework before the therapist can practice dry needling in this state.
(5) Dry needling may only be performed by a licensed physical therapist and may not be delegated to a physical therapist assistant or support personnel.
(6) A physical therapist practicing dry needling must supply written documentation, upon request by the Board, that substantiates appropriate training as required by this rule. (7) All physical therapy patients receiving dry needling for the first time shall be provided written documentation from the patient’s physical therapist that includes a definition and description of the practice of dry needling, a description of the education and training taken by the physical therapist which qualifies the therapist to practice dry needling, and a description of any potential side effects of dry needling, and the patient must give written informed consent after acknowledging the risks before dry needling may begin.
In January 2008, the Texas Board of Physical Therapy Examiners determined that dry needling is within the scope of physical therapy practice. TX allows PT to take DN Courses and currently they do not have any specific credential hours-requirements, but they said that it is the responsibility of the Licensee to make sure that he/she is competent enough to incorporate DN in their practice and use it safely.
On April 1: Utah Governor Gary R. Herbert signed into law HB 367. The legislation amends the Utah physical therapy statute to specifically add dry needling to the physical therapist scope of practice.
On June 22, 2015, the Office of Regulation replied pointing out that “under the existing law, the Vermont Office of Professional Regulation believes that physical therapists reasonably may practice TDN if appropriately trained and experienced, and if the therapy is reasonably indicated for the relief of an impairment of physical movement.”
Guidance Document 112-9
Board of Physical Therapy Guidance on Dry Needling in the Practice of Physical Therapy Upon recommendation from the Task Force on Dry Needling, the board voted that dry needling is within the scope of practice of physical therapy
Learn about our new 3-course package to achieve your states requirement HERE.
Effective July 2023: Washington approved Dry Needling for Physical Therapist. Dry Needling Rules
In July 2012 the West Virginia Board of Physical Therapy issued its “Opinion regarding Dry Needling Therapy” and concluded that dry needling is within the scope of practice of “physical therapy”.
In July 2009, the Wisconsin Physical Therapy Affiliated Credentialing Board determined trigger point dry needling as within the scope of practice of physical therapy provided that the licensed physical therapist is properly educated and trained.
In a letter dated Aug 18 2009: the Wyoming Board of Physical Therapy affirmed that nothing in the current practice act would preclude PTs performing dry needling with proper credentials.
Section 3. Evidence of competence; dry needling.
(a) Dry needling may not be performed by a PTA or a physical therapy aide.
(b) Licensed physical therapists shall demonstrate that they have received training in dry needling in a course approved by state boards of physical therapy, the American Physical Therapy Association or individual chapters of the American Physical Therapy Association, the Federation of State Boards of Physical Therapy, or the International Association for Continuing 7-3
Education Training.
(i) The course shall include but not be limited to training in indications, contraindications, potential risks, proper hygiene, proper use and disposal of needles, and appropriate selection of clients.
(ii) The course shall include a minimum of twenty-seven (27) hours of live face-to-face instruction. Online courses are not appropriate training in dry needling.
(c) The physical therapist shall supply written documentation, upon request by the Board, that substantiates appropriate training as required by this rule. Failure to provide written documentation may result in disciplinary action taken by the Board.
The Connecticut Board of Examiners has not ruled for or against physical therapists performing dry needling.
The Massachusetts Board of Allied Health Professionals has not formally ruled on dry needling by physical therapists.
The Michigan Board of Physical Therapy has not formally ruled on dry needling by physical therapists.
The Minnesota Board of Physical Therapy is prohibited from issuing advisory opinions or position statements. Therefore, there is no formal ruling on dry needling by physical therapists.
The Missouri Board of Registration for the Healing Arts (Advisory Commission for Physical Therapists) has not formally ruled on dry needling by physical therapists.
The Oklahoma Medical Board Physical Therapists Committee has not formally ruled on dry needling by physical therapists.
Currently it remains undetermined whether dry needling is within the scope of PT practice in Pennsylvania.
Dry Needling is prohibited in CA.
In Hawaii, physical therapists are not allowed to penetrate the skin and therefore dry needling is not within the scope of PT practice.
In 1992, the New York Board of Education concluded that dry needling would not be allowed by physical therapists.
On May 17, 2017, the Attorney General of Oregon issued a statement that dry needling is not within the scope of practice of a physical therapist licensed in Oregon.

© Integrative Dry Needling 2025 | All rights reserved | Designed by Weblink
any IDN Course!
*Valid for new registrations only and can not be combined with other discount codes. Offer Expires: 7/7/2024

Not sure which course is right for you? No problem – we created an intuitive process to help!